The Silent Epidemic: Why Oral Care Matters for Your Pet
For many pet owners, the focus of their pet’s health routine centers around annual vaccinations, parasite control, and high-quality food. Yet, one critical aspect is frequently overlooked until a serious problem arises: dental care. Periodontal disease, the gradual destruction of the tissue surrounding the teeth, is the most common clinical condition affecting adult dogs and cats.
Shockingly, studies indicate that by the age of three, over 80% of dogs and 70% of cats exhibit signs of dental disease. This pervasive issue is not just about bad breath; it’s a gateway to systemic health problems that can significantly shorten a pet’s lifespan and diminish their quality of life. This extensive guide dives into the anatomy, pathology, consequences, and best practices for ensuring your beloved companion maintains a healthy, pain-free smile.
Anatomical Foundations: Understanding Your Pet’s Mouth
To truly appreciate the necessity of dental care, it is vital to understand the basic structure of your pet’s oral cavity. Unlike humans who have two sets of teeth, dogs and cats follow a similar pattern: deciduous (baby) teeth followed by permanent teeth.
A. Canine Dental Formula: An adult dog typically possesses 42 permanent teeth. This formula is specialized for their scavenging and tearing needs, featuring large, pointed canines for grasping and powerful, shearing cheek teeth (premolars and molars), with the upper fourth premolar and lower first molar forming the critical carnassial teeth used for slicing meat and crushing bone.
B. Feline Dental Formula: Adult cats have a more streamlined set of 30 permanent teeth, reflecting their status as obligate carnivores. Their teeth are sharper and more pointed, focusing almost entirely on cutting and shearing with very little surface area for grinding, making them highly efficient hunters.
C. The Periodontium: This term refers to the specialized tissues that support the tooth in the jawbone. It includes the gingiva (gums), the cementum (layer covering the tooth root), the periodontal ligament (which attaches the tooth to the bone), and the alveolar bone (the jawbone itself). When dental disease strikes, it is this entire supporting structure that is targeted for destruction.
The Progression of Periodontal Disease: From Plaque to Pain
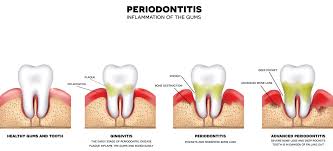
Dental disease is not an overnight occurrence; it is a gradual, insidious process driven by the persistent accumulation of bacteria. Understanding the stages is key to recognizing the problem early.
Stage 1: Plaque Formation (Gingivitis)
Immediately after a professional cleaning or a meal, bacteria begin colonizing the tooth surface, creating a sticky, invisible film called plaque.
A. Bacterial Biofilm: Plaque is a complex, active community of microorganisms, glycoproteins from saliva, and food debris. If not removed within hours, these bacteria initiate an inflammatory response in the adjacent gums.
B. Gingivitis: This is the first, reversible stage of periodontal disease. The gums become red, swollen, and may bleed easily, but there is no irreversible damage to the underlying bone or ligaments yet. Regular brushing can completely resolve gingivitis.
Stage 2: Calculus (Tartar) Development
If plaque remains undisturbed, mineral salts present in the saliva react with the plaque, leading to its calcification.
A. Tartar Hardening: Within 24-72 hours, plaque starts to mineralize into a hard, cement-like substance called calculus or tartar. Tartar provides a rough surface that attracts and retains even more plaque, accelerating the disease.
B. Irreversible Damage Begins: The mechanical irritation from the tartar and the toxins released by the subgingival (below the gumline) bacteria begin to damage the periodontal ligament and alveolar bone.
Stage 3 & 4: Periodontitis and Bone Loss
As the process continues, the disease progresses into periodontitis, which is characterized by the irreversible destruction of the tooth’s supporting structures.
A. Pocket Formation: The inflammation causes the gum tissue to detach from the tooth root, forming a space known as a periodontal pocket. These deep, anaerobic (low-oxygen) pockets become breeding grounds for the most destructive types of bacteria.
B. Alveolar Bone Resorption: The body’s immune response, intended to fight the bacteria, releases inflammatory mediators (e.g., matrix metalloproteinases) that inadvertently destroy the bone supporting the tooth. This leads to bone loss, receding gums, and eventual tooth mobility.
C. Advanced Disease: In the final stages, severe bone loss occurs, the tooth becomes very loose, and pain is significant. Pathological jaw fracture can even occur in small breeds where advanced periodontal disease has destroyed a large portion of the mandibular (jaw) bone around the canine teeth.
The Systemic Consequences: Beyond the Mouth
Ignoring your pet’s dental health is equivalent to ignoring a chronic, low-grade infection constantly circulating through their body. The toxins and bacteria from the inflamed periodontal tissues can enter the bloodstream (a condition known as bacteremia) and travel to distant organs.
1. Cardiovascular Disease
A. Bacterial Endocarditis: Bacteria from the mouth can settle on the heart valves, causing inflammation and damage to the lining of the heart (endocarditis). Over time, this can lead to thickening and functional impairment of the valves, potentially contributing to congestive heart failure. Pets with pre-existing heart murmurs are particularly vulnerable.
2. Kidney and Liver Damage
A. Organ Filtration Stress: The kidneys and liver are the body’s main filtration and detoxification systems. They are constantly exposed to bacterial toxins and immune complexes carried in the bloodstream from the dental infection. Over years, this chronic burden can contribute to or exacerbate the progression of chronic kidney disease and liver inflammation, two leading causes of morbidity and mortality in older pets.
3. Diabetes Mellitus Management
A. Inflammatory Link: Chronic infection and inflammation, such as that caused by severe periodontitis, can increase insulin resistance in the body. This makes it significantly more challenging to regulate blood glucose levels in diabetic pets, often requiring higher or less stable doses of insulin. Treating the underlying dental disease is a critical step in achieving successful diabetes management.
4. Chronic Pain and Quality of Life
A. Hidden Suffering: Pets are masters at hiding chronic pain, especially oral pain. Owners often mistake their pet slowing down, becoming grumpy, or changing their chewing habits as simply “getting old.” However, severe periodontitis is excruciating. When the pain is resolved through dental treatment, owners frequently report a dramatic return of playfulness, better appetite, and increased energy, demonstrating how much pain the pet was silently enduring.
Professional Veterinary Dental Care (COHAT)
While home care is essential for maintenance, only a veterinarian can address the disease that already exists below the gumline. This requires a procedure known as a Comprehensive Oral Assessment and Treatment (COHAT).
The Necessity of Anesthesia
Many owners are hesitant about anesthesia, but for pets, it is the only way to perform a proper dental cleaning and assessment.
A. Safety and Monitoring: Modern veterinary anesthesia protocols are highly sophisticated and safe. They involve thorough pre-anesthetic blood work, intravenous catheter placement, and continuous monitoring of vitals (heart rate, respiration, blood pressure, oxygen saturation) by a dedicated veterinary nurse or technician.
B. Subgingival Cleaning: The most critical part of dental disease is below the gumline. A pet cannot tolerate the necessary scraping (scaling) and root planing required to remove tartar from the roots without being immobile under general anesthesia.
C. Complete Oral Exam: Anesthesia allows the veterinarian to thoroughly probe every tooth surface and check for hidden problems like fractured teeth, pockets, and feline odontoclastic resorptive lesions (FORLs)—painful “holes” that commonly form in cats’ teeth.
Key Steps in a COHAT Procedure
A. Supragingival and Subgingival Scaling: Using specialized ultrasonic scalers and hand instruments to remove all plaque and calculus from above and below the gumline.
B. Dental Radiography (X-rays): This is perhaps the most crucial step. Up to 60% of dental disease is hidden beneath the gums. X-rays reveal bone loss, abscesses, unerupted teeth, and root damage. A dental cleaning without X-rays is considered substandard care.
C. Polishing: Scaling leaves microscopic scratches on the enamel, which trap plaque. Polishing smooths these surfaces, making it harder for bacteria to adhere.
D. Periodontal Treatments or Extractions: Teeth with severe periodontitis (usually Grade 3 or 4), deep periodontal pockets, or irreversible damage may require advanced treatments or, most often, extraction to resolve the infection and eliminate the source of chronic pain.
Establishing an Effective Home Dental Care Routine

Professional cleanings treat the existing disease, but home care is the absolute cornerstone of prevention. Once the teeth are clean, the owner’s job is to keep them clean.
1. Brushing: The Gold Standard
Daily tooth brushing is the most effective way to mechanically disrupt and remove plaque before it hardens into tartar.
A. Technique and Tools: Use a soft-bristled toothbrush or a finger brush designed for pets. Crucially, use veterinary-approved pet toothpaste. Human toothpaste contains fluoride, detergents, and foaming agents that are toxic if swallowed, which pets inevitably do. Pet toothpaste comes in flavors like chicken or beef, making the process more palatable.
B. Focus on the Outside: Focus primarily on the outer (buccal) surfaces of the teeth. Plaque accumulates fastest here due to the proximity to the salivary ducts, and the pet’s tongue naturally cleans the inner surface somewhat.
C. Consistency is Key: Aim for brushing every day. Plaque mineralizes in under three days, so brushing at least every other day is the minimum frequency to be effective. Start gradually, allowing the pet to lick the toothpaste first, then slowly introducing the brush.
2. Dietary and Chewing Aids
While no dental product is as effective as brushing, certain products can aid in plaque control.
A. Veterinary Oral Health Council (VOHC) Approved Products: Look for the VOHC Seal of Acceptance on chews, water additives, and diets. This seal means the product has undergone clinical trials proving it reduces plaque and/or tartar by at least a specified margin. Products without this seal are often ineffective.
B. Dental Diets: Specialty veterinary dental diets are formulated with an altered fiber matrix or a specific coating (e.g., sodium hexametaphosphate) that mechanically scrubs the tooth as the pet chews or chemically binds with calcium in the saliva to inhibit tartar formation.
C. Safe Chews: Rawhide, vegetable-based chews, and certain dental toys can provide mechanical abrasion. Avoid non-flexible objects like bones, antlers, or ice cubes, which can easily cause the painful slab fractures mentioned earlier. If you cannot easily dent or break the chew with your hands, it is likely too hard for your pet’s teeth (the “thumb test”).
3. Other Aids
A. Oral Rinses and Gels: Products containing chlorhexidine (an antiseptic) can be applied to the gums to reduce the bacterial count, particularly useful for pets that absolutely cannot tolerate brushing.
B. Water Additives: These typically contain ingredients intended to reduce bacteria in the mouth or inhibit the formation of tartar. They are a passive, easy solution, but their efficacy is limited and often best used as an adjunct to brushing, not a replacement.
Dispelling Common Dental Myths
The dental health space is rife with misinformation that can unintentionally harm a pet’s health.
Myth 1: Hard Kibble Cleans Teeth
This is one of the most persistent myths. Standard kibble shatters upon impact, often providing little to no mechanical cleaning action, especially against the gumline where the plaque accumulates. Only specially formulated, VOHC-approved dental diets have proven plaque-reducing benefits.
Myth 2: Anesthesia-Free Dentals are Safe and Effective
This practice, often performed by non-veterinarians, is misleading and dangerous. A.F.D.s (Anesthesia-Free Dentals) only clean the surface of the tooth (cosmetic cleaning) and cannot access the subgingival area where the disease actually occurs. Furthermore, without X-rays, any hidden pathology is missed. Because the pet is awake, the procedure is stressful and often painful, and the sharp instruments can easily injure the pet or the operator. The American Veterinary Dental College (AVDC) and the American Veterinary Medical Association (AVMA) strongly condemn this practice.
Myth 3: Bad Breath is Normal for an Old Pet
While common, halitosis (bad breath) is a clinical sign of active infection and disease, not a normal part of aging. It is caused by volatile sulfur compounds produced by anaerobic bacteria in the mouth. Bad breath is a signal that your pet is in need of professional veterinary attention.
Lifetime Dental Wellness Planning
Good dental health is not a one-time fix; it’s a commitment for the duration of your pet’s life.
A. Puppy/Kittenhood: Start handling your pet’s mouth early and introduce gentle tooth brushing without paste to desensitize them. Monitor for retained deciduous teeth (baby teeth that don’t fall out), which are common in small dogs and can cause crowding, necessitating removal around 5-6 months of age, often during the spay/neuter surgery.
B. Adulthood (Ages 1-7): Establish the daily brushing routine. Most adult pets require professional COHAT procedures every 1 to 3 years, depending on their individual propensity for plaque accumulation. Genetic factors play a huge role; some breeds (e.g., Yorkshire Terriers, Maltese, Greyhounds) require annual cleanings.
C. Senior Years (Ages 7+): Increased vigilance is required. Senior pets often have more advanced disease and require thorough pre-anesthetic testing, but the pain relief from addressing the dental issues significantly improves their twilight years.
Economic Impact and Long-Term Savings
While a professional dental cleaning under anesthesia can seem expensive, it is a crucial investment that often saves significantly more money—and prevents immense suffering—in the long run. Preventive care avoids the much higher costs associated with:
A. Multi-Tooth Extractions: Removing severely diseased teeth requires complex surgery, local nerve blocks, and post-operative pain management.
B. Systemic Disease Management: Treating conditions like severe kidney failure or poorly managed diabetes, which have been exacerbated by chronic dental infection, is far more costly and challenging than addressing the root cause.
C. Emergency Procedures: Repairing a fractured jaw or treating a life-threatening osteomyelitis (bone infection) stemming from a tooth abscess.
Conclusion
The pervasive nature of periodontal disease in pets underscores a critical gap in owner awareness. Pet ownership involves accepting responsibility for all aspects of their well-being, and oral health cannot be relegated to an afterthought. A healthy mouth is inextricably linked to a healthy body. By committing to a partnership between consistent home care (especially daily brushing) and regular, comprehensive professional veterinary assessments (including dental X-rays), you are not just eliminating bad breath; you are actively extending your pet’s healthspan, protecting their vital organs, and ensuring their final years are spent in comfort, not chronic pain. Don’t ignore the silent plea for dental care—your pet’s quality of life depends on it.